Search
- Page Path
- HOME > Search
- Household secondary attack rates and risk factors during periods of SARS-CoV-2 Delta and Omicron variant predominance in the Republic of Korea
- Jin Lee, Mijeong Ko, Seontae Kim, Dosang Lim, Gemma Park, Sang-Eun Lee
- Osong Public Health Res Perspect. 2023;14(4):263-271. Published online August 11, 2023
- DOI: https://doi.org/10.24171/j.phrp.2023.0133
- 1,890 View
- 133 Download
-
 Graphical Abstract
Graphical Abstract
 Abstract
Abstract
 PDF
PDF 
- Objectives
The household secondary attack rate (SAR) of severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) is an important indicator for community transmission. This study aimed to characterize transmission by comparing household SARs and identifying risk factors during the periods of Delta and Omicron variant predominance in Republic of Korea.
Methods
We defined the period of Delta variant predominance (Delta period) as July 25, 2021 to January 15, 2022, and the period of Omicron variant predominance (Omicron period) as February 7 to September 3, 2022. The number of index cases included was 214,229 for the Delta period and 5,521,393 for the Omicron period. To identify the household SARs and risk factors for each period, logistic regression was performed to determine the adjusted odds ratio (aOR).
Results
The SAR was 35.2% for the Delta period and 43.1% for the Omicron period. The aOR of infection was higher in 2 groups, those aged 0 to 18 years and ≥75 years, compared to those aged 19 to 49 years. Unvaccinated individuals (vs. vaccinated individuals) and individuals experiencing initial infection (vs. individuals experiencing a second or third infection) had an increased risk of infection with SARS-CoV-2.
Conclusion
This study analyzed the household SARs and risk factors. We hope that the results can help develop age-specific immunization plans and responses to reduce the SAR in preparation for emerging infectious diseases or potential new variants of SARS-CoV-2.
- Increased viral load in patients infected with severe acute respiratory syndrome coronavirus 2 Omicron variant in the Republic of Korea
- Jeong-Min Kim, Dongju Kim, Nam-Joo Lee, Sang Hee Woo, Jaehee Lee, Hyeokjin Lee, Ae Kyung Park, Jeong-Ah Kim, Chae Young Lee, Il-Hwan Kim, Cheon Kwon Yoo, Eun-Jin Kim
- Osong Public Health Res Perspect. 2023;14(4):272-278. Published online July 27, 2023
- DOI: https://doi.org/10.24171/j.phrp.2023.0024
- 1,328 View
- 108 Download
-
 Graphical Abstract
Graphical Abstract
 Abstract
Abstract
 PDF
PDF 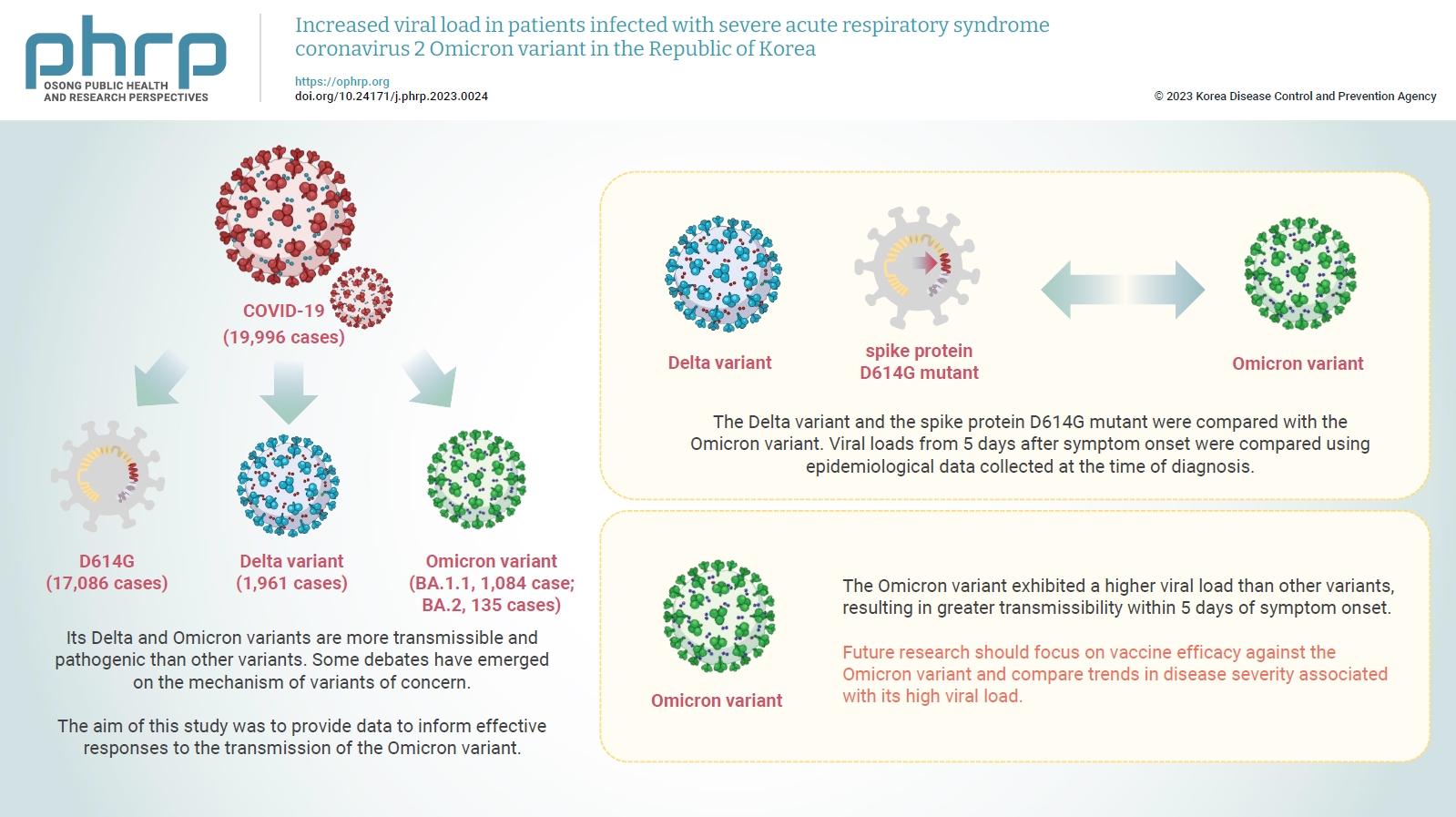
- Objectives
Coronavirus disease 2019 (COVID-19) has been declared a global pandemic owing to the rapid spread of the causative agent, severe acute respiratory syndrome coronavirus 2. Its Delta and Omicron variants are more transmissible and pathogenic than other variants. Some debates have emerged on the mechanism of variants of concern. In the COVID-19 wave that began in December 2021, the Omicron variant, first reported in South Africa, became identifiable in most cases globally. The aim of this study was to provide data to inform effective responses to the transmission of the Omicron variant.
Methods
The Delta variant and the spike protein D614G mutant were compared with the Omicron variant. Viral loads from 5 days after symptom onset were compared using epidemiological data collected at the time of diagnosis.
Results
The Omicron variant exhibited a higher viral load than other variants, resulting in greater transmissibility within 5 days of symptom onset.
Conclusion
Future research should focus on vaccine efficacy against the Omicron variant and compare trends in disease severity associated with its high viral load.
- 2019 Tabletop Exercise for Laboratory Diagnosis and Analyses of Unknown Disease Outbreaks by the Korea Centers for Disease Control and Prevention
- Il-Hwan Kim, Jun Hyeong Jang, Su-Kyoung Jo, Jin Sun No, Seung-Hee Seo, Jun-Young Kim, Sang-Oun Jung, Jeong-Min Kim, Sang-Eun Lee, Hye-Kyung Park, Eun-Jin Kim, Jun Ho Jeon, Myung-Min Choi, Boyeong Ryu, Yoon Suk Jang, Hwami Kim, Jin Lee, Seung-Hwan Shin, Hee Kyoung Kim, Eun-Kyoung Kim, Ye Eun Park, Cheon-Kwon Yoo, Sang-Won Lee, Myung-Guk Han, Gi-Eun Rhie, Byung Hak Kang
- Osong Public Health Res Perspect. 2020;11(5):280-285. Published online October 22, 2020
- DOI: https://doi.org/10.24171/j.phrp.2020.11.5.03
- 5,862 View
- 106 Download
-
 Abstract
Abstract
 PDF
PDF Objectives The Korea Centers for Disease Control and Prevention has published “A Guideline for Unknown Disease Outbreaks (UDO).” The aim of this report was to introduce tabletop exercises (TTX) to prepare for UDO in the future.
Methods The UDO Laboratory Analyses Task Force in Korea Centers for Disease Control and Prevention in April 2018, assigned unknown diseases into 5 syndromes, designed an algorithm for diagnosis, and made a panel list for diagnosis by exclusion. Using the guidelines and laboratory analyses for UDO, TTX were introduced.
Results Since September 9th, 2018, the UDO Laboratory Analyses Task Force has been preparing TTX based on a scenario of an outbreak caused by a novel coronavirus. In December 2019, through TTX, individual missions, epidemiological investigations, sample treatments, diagnosis by exclusions, and next generation sequencing analysis were discussed, and a novel coronavirus was identified as the causal pathogen.
Conclusion Guideline and laboratory analyses for UDO successfully applied in TTX. Conclusions drawn from TTX could be applied effectively in the analyses for the initial response to COVID-19, an ongoing epidemic of 2019 – 2020. Therefore, TTX should continuously be conducted for the response and preparation against UDO.
- Development and Utilization of a Rapid and Accurate Epidemic Investigation Support System for COVID-19
- Young Joon Park, Sang Yun Cho, Jin Lee, Ikjin Lee, Won-Ho Park, Seungmyeong Jeong, Seongyun Kim, Seokjun Lee, Jaeho Kim, Ok Park
- Osong Public Health Res Perspect. 2020;11(3):118-127. Published online May 20, 2020
- DOI: https://doi.org/10.24171/j.phrp.2020.11.3.06
- 12,572 View
- 302 Download
- 22 Web of Science
- 23 Crossref
-
 Abstract
Abstract
 PDF
PDF Objectives In this pandemic situation caused by a novel coronavirus disease in 2019 (COVID-19), an electronic support system that can rapidly and accurately perform epidemic investigations, is needed. It would systematically secure and analyze patients’ data (who have been confirmed to have the infection), location information, and credit card usage.
Methods The “Infectious Disease Prevention and Control Act” in South Korea, established a legal basis for the securement, handling procedure, and disclosure of information required for epidemic investigations. The Epidemic Investigation Support System (EISS) was developed as an application platform on the Smart City data platform.
Results The EISS performed the function of inter-institutional communication which reduced the processing period of patients’ data in comparison to other methods. This system automatically marked confirmed cases’ tracking data on a map and hot-spot analysis which lead to the prediction of areas where people may be vulnerable to infection.
Conclusion The EISS was designed and implemented for use during an epidemic investigation to prevent the spread of an infectious disease, by specifically tracking confirmed cases of infection.
-
Citations
Citations to this article as recorded by- The Birth of Digital Epidemiology in South Korea
Eun-Sung Kim
East Asian Science, Technology and Society: An Int.2024; 18(1): 22. CrossRef - Modern technologies and solutions to enhance surveillance and response systems for emerging zoonotic diseases
Li Zhang, Wenqiang Guo, Chenrui Lv
Science in One Health.2024; 3: 100061. CrossRef - Within-Host Evolution of SARS-CoV-2 in a B-Cell Depleted Patient With Successful Treatment
Yae Jee Baek, Gemma Park, Jun Yong Choi, Eun Jin Kim, Bryan Inho Kim, Jin Gwack, Ji Ye Jung
Journal of Korean Medical Science.2023;[Epub] CrossRef - Contact-tracing of the COVID-19 spreading using digital technologies with artificial intelligence (literary review)
Botir T. Daminov, Sherzod P. Ashirbaev, Igor P. Vikhrov
HEALTH CARE OF THE RUSSIAN FEDERATION.2023; 67(2): 142. CrossRef - 엠폭스(원숭이두창)의 효과적 관리 방안: 역학조사 경험과 국외 정책 검토
태영 김, 언주 박, 종무 김, 민결 심, 신영 이, 은경 김
Public Health Weekly Report.2023; 16(22): 669. CrossRef - Epidemiological analysis of coronavirus disease (COVID-19) patients on ships arriving at Busan port in Korea, 2020
Kee Hun Do, Jinseon Yang, Ok Sook Do, Seok-Ju Yoo, Rajnesh Lal
PLOS ONE.2023; 18(7): e0288064. CrossRef - IntelliTrace: Intelligent Contact Tracing Method Based on Transmission Characteristics of Infectious Disease
Soorim Yang, Kyoung-Hwan Kim, Hye-Ryeong Jeong, Seokjun Lee, Jaeho Kim
Applied System Innovation.2023; 6(6): 112. CrossRef - Detecting mpox infection in the early epidemic: an epidemiologic investigation of the third and fourth cases in Korea
Taeyoung Kim, Eonjoo Park, Jun Suk Eun, Eun-young Lee, Ji Won Mun, Yunsang Choi, Shinyoung Lee, Hansol Yeom, Eunkyoung Kim, Jongmu Kim, Jihyun Choi, Jinho Ha, Sookkyung Park
Epidemiology and Health.2023; 45: e2023040. CrossRef - A scalable framework for smart COVID surveillance in the workplace using Deep Neural Networks and cloud computing
Ajay Singh, Vaibhav Jindal, Rajinder Sandhu, Victor Chang
Expert Systems.2022;[Epub] CrossRef - COVID-19 Cluster Linked to Aerosol Transmission of SARS-CoV-2 via Floor Drains
Taewon Han, Heedo Park, Yungje Jeong, Jungmin Lee, Eungyeong Shon, Man-Seong Park, Minki Sung
The Journal of Infectious Diseases.2022; 225(9): 1554. CrossRef - Perceived usefulness of COVID-19 tools for contact tracing among contact tracers in Korea
Seonyeong Gong, Jong Youn Moon, Jaehun Jung
Epidemiology and Health.2022; 44: e2022106. CrossRef - Public health in times of crisis: An overlooked variable in city management theories?
Celso Machado, Daielly Melina Nassif Mantovani Ribeiro, Adriana Backx Noronha Viana
Sustainable Cities and Society.2021; 66: 102671. CrossRef - Re-estimation of basic reproduction number of COVID-19 based on the epidemic curve by symptom onset date
K. Hong, S. J. Yum, J. H. Kim, B. C. Chun
Epidemiology and Infection.2021;[Epub] CrossRef - Benefits of Mobile Contact Tracing on COVID-19: Tracing Capacity Perspectives
Uichin Lee, Auk Kim
Frontiers in Public Health.2021;[Epub] CrossRef - Two-Way Contact Network Modeling for Identifying the Route of COVID-19 Community Transmission
Sung Jin Lee, Sang Eun Lee, Ji-On Kim, Gi Bum Kim
Informatics.2021; 8(2): 22. CrossRef - State of the Art in Adoption of Contact Tracing Apps and Recommendations Regarding Privacy Protection and Public Health: Systematic Review
Katarzyna Kolasa, Francesca Mazzi, Ewa Leszczuk-Czubkowska, Zsombor Zrubka, Márta Péntek
JMIR mHealth and uHealth.2021; 9(6): e23250. CrossRef - Riding the waves of the COVID-19 pandemic in South Korea
Joseph Christian Obnial, Maria Beatriz Baron, Hannah Andrea Sagsagat, Erika Ong, Ma. Alexandra Nicola Valenzuela, Don Eliseo Lucero-Prisno
Journal of Primary Health Care.2021; 13(2): 116. CrossRef - Contributions of Smart City Solutions and Technologies to Resilience against the COVID-19 Pandemic: A Literature Review
Ayyoob Sharifi, Amir Reza Khavarian-Garmsir, Rama Krishna Reddy Kummitha
Sustainability.2021; 13(14): 8018. CrossRef - Harnessing the Power of Smart and Connected Health to Tackle COVID-19: IoT, AI, Robotics, and Blockchain for a Better World
Farshad Firouzi, Bahar Farahani, Mahmoud Daneshmand, Kathy Grise, Jaeseung Song, Roberto Saracco, Lucy Lu Wang, Kyle Lo, Plamen Angelov, Eduardo Soares, Po-Shen Loh, Zeynab Talebpour, Reza Moradi, Mohsen Goodarzi, Haleh Ashraf, Mohammad Talebpour, Alireza
IEEE Internet of Things Journal.2021; 8(16): 12826. CrossRef - CASE-CF: Context Aware Smart Epidemic Control Framework
Harsuminder Kaur Gill, Vivek Kumar Sehgal, Anil Kumar Verma
New Generation Computing.2021; 39(3-4): 541. CrossRef - Resolving the tension between full utilization of contact tracing app services and user stress as an effort to control the COVID-19 pandemic
Jaehun Joo, Matthew Minsuk Shin
Service Business.2020; 14(4): 461. CrossRef - National Disaster Management System: COVID-19 Case in Korea
Junic Kim, Kelly Ashihara
International Journal of Environmental Research an.2020; 17(18): 6691. CrossRef - Evidence of Long-Distance Droplet Transmission of SARS-CoV-2 by Direct Air Flow in a Restaurant in Korea
Keun-Sang Kwon, Jung-Im Park, Young Joon Park, Don-Myung Jung, Ki-Wahn Ryu, Ju-Hyung Lee
Journal of Korean Medical Science.2020;[Epub] CrossRef
- The Birth of Digital Epidemiology in South Korea
- Corrigendum to “Exposure to Dichlorodiphenyltrichloroethane and the Risk of Breast Cancer: A Systematic Review and Meta-analysis [Volume 5, Issue 2, April 2014, Pages 77–84]”
- Jae-Hong Park, Eun Shil Cha, Yousun Ko, Myung-Sil Hwang, Jin-Hwan Hong, Won Jin Lee
- Osong Public Health Res Perspect. 2015;6(4):279-279. Published online August 31, 2015
- DOI: https://doi.org/10.1016/j.phrp.2015.07.004
- 2,608 View
- 16 Download
- Exposure to Dichlorodiphenyltrichloroethane and the Risk of Breast Cancer: A Systematic Review and Meta-analysis
- Jae-Hong Park, Eun Shil Cha, Yousun Ko, Myung-Sil Hwang, Jin-Hwan Hong, Won Jin Lee
- Osong Public Health Res Perspect. 2014;5(2):77-84. Published online April 30, 2014
- DOI: https://doi.org/10.1016/j.phrp.2014.02.001
- 3,293 View
- 26 Download
- 24 Crossref
-
 Abstract
Abstract
 PDF
PDF - Objectives
This study extended and updated a meta-analysis of the association between exposure to dichlorodiphenyltrichloroethane (DDT) and the risk of breast cancer.
Methods
We reviewed the published literature on exposure to DDE and breast cancer risk to update a meta-analysis from 2004. The total of 35 studies included 16 hospital-based case–control studies, 11 population-based case–control studies, and 10 nested case–control studies identified through keyword searches in the PubMed and EMBASE databases.
Results
The summary odds ratio (OR) for the identified studies was 1.03 (95% confidence interval 0.95–1.12) and the overall heterogeneity in the OR was observed (I2 = 40.9; p = 0.006). Subgroup meta-analyses indicated no significant association between exposure to DDE and breast cancer risk by the type of design, study years, biological specimen, and geographical region of the study, except from population-based case–control studies with estimated DDE levels in serum published in 1990s.
Conclusion
Existing studies do not support the view that DDE increases the risk of breast cancer in humans. However, further studies incorporating more detailed information on DDT exposure and other potential risk factors for breast cancer are needed. -
Citations
Citations to this article as recorded by- Causes and Risk Factors of Breast Cancer, What Do We Know for Sure? An Evidence Synthesis of Systematic Reviews and Meta-Analyses
Borghild Løyland, Ida Hellum Sandbekken, Ellen Karine Grov, Inger Utne
Cancers.2024; 16(8): 1583. CrossRef - Validation and green profile assessment of a binary solvent liquid phase microextraction method for the determination of chlorbenside and fenobucarb in lake and wastewater samples by GC–MS
Dotse Selali Chormey
Environmental Science and Pollution Research.2023; 30(15): 44697. CrossRef - Putative interactions between transthyretin and endosulfan II and its relevance in breast cancer
Saurabh Sharma, Lakshay Malhotra, Paromita Mukherjee, Navneet Kaur, Thammineni Krishanlata, Chittur V. Srikanth, Vandana Mishra, Basu Dev Banerjee, Abdul Samath Ethayathulla, Radhey Shyam Sharma
International Journal of Biological Macromolecules.2023; 235: 123670. CrossRef - Exposure to Organochlorine Pesticides and Female Breast Cancer Risk According to Molecular Receptors Expression: a Systematic Review and Meta-analysis of Epidemiological Evidence
Rodrigo Ugalde-Resano, Brenda Gamboa-Loira, Ángel Mérida-Ortega, Alma Rincón-Rubio, Gisela Flores-Collado, Maricela Piña-Pozas, Lizbeth López-Carrillo
Current Environmental Health Reports.2023; 10(4): 442. CrossRef - Mosquito control exposures and breast cancer risk: analysis of 1071 cases and 2096 controls from the Ghana Breast Health Study
Naomie Olivos, Jim E. Banta, Rhonda Spencer-Hwang, Daniel Ansong, Laura E. Beane Freeman, Joe-Nat Clegg-Lamptey, Beatrice Wiafe-Addai, Lawrence Edusei, Ernest Adjei, Nicholas Titiloye, Florence Dedey, Francis Aitpillah, Joseph Oppong, Verna Vanderpuye, Er
Breast Cancer Research.2023;[Epub] CrossRef - Endocrine disrupting chemicals and breast cancer: a systematic review of epidemiological studies
Murphy Lam Yim Wan, Vanessa Anna Co, Hani El-Nezami
Critical Reviews in Food Science and Nutrition.2022; 62(24): 6549. CrossRef - Epidemiology beyond its limits
Lauren E. McCullough, Maret L. Maliniak, Avnika B. Amin, Julia M. Baker, Davit Baliashvili, Julie Barberio, Chloe M. Barrera, Carolyn A. Brown, Lindsay J. Collin, Alexa A. Freedman, David C. Gibbs, Maryam B. Haddad, Eric W. Hall, Sarah Hamid, Kristin R. V
Science Advances.2022;[Epub] CrossRef - Plasma concentrations of chlorinated persistent organic pollutants and their predictors in the general population of Algiers, Algeria
El Hadia Mansouri, Mohamed Reggabi
Emerging Contaminants.2021; 7: 35. CrossRef - Association between type 2 diabetes and exposure to chlorinated persistent organic pollutants in Algeria: A case-control study
El Hadia Mansouri, Mohamed Reggabi
Chemosphere.2021; 264: 128596. CrossRef - Extraction of Chlorobenzenes and PCBs from Water by ZnO Nanoparticles
Yuntao Zhang, Ran Chen, Jim E. Riviere, Jeffrey Comer
Processes.2021; 9(10): 1764. CrossRef - Two Cases of Possible Familial Chronic Myeloid Leukemia in a Family with Extensive History of Cancer
Marisa J.L. Aitken, Christopher B. Benton, Ghayas C. Issa, Koji Sasaki, Musa Yilmaz, Nicholas J. Short
Acta Haematologica.2021; 144(5): 585. CrossRef - In utero DDT exposure and breast density before age 50
Nickilou Y. Krigbaum, Piera M. Cirillo, Julie D. Flom, Jasmine A. McDonald, Mary Beth Terry, Barbara A. Cohn
Reproductive Toxicology.2020; 92: 85. CrossRef - DDT exposure during pregnancy and DNA methylation alterations in female offspring in the Child Health and Development Study
Hui-Chen Wu, Barbara A. Cohn, Piera M. Cirillo, Regina M. Santella, Mary Beth Terry
Reproductive Toxicology.2020; 92: 138. CrossRef - Prediagnostic serum concentrations of organochlorine pesticides and non-Hodgkin lymphoma: A nested case–control study in the Norwegian Janus Serum Bank Cohort
Dazhe Chen, Tom K. Grimsrud, Hilde Langseth, Dana B. Barr, Bryan A. Bassig, Aaron Blair, Kenneth P. Cantor, Marilie D. Gammon, Qing Lan, Nathaniel Rothman, Lawrence S. Engel
Environmental Research.2020; 187: 109515. CrossRef - Global trends in pesticides: A looming threat and viable alternatives
Akanksha Sharma, Ananya Shukla, Kriti Attri, Megha Kumar, Puneet Kumar, Ashish Suttee, Gurpal Singh, Ravi Pratap Barnwal, Neha Singla
Ecotoxicology and Environmental Safety.2020; 201: 110812. CrossRef - Exposure to Endocrine Disrupting Chemicals and Risk of Breast Cancer
Louisane Eve, Béatrice Fervers, Muriel Le Romancer, Nelly Etienne-Selloum
International Journal of Molecular Sciences.2020; 21(23): 9139. CrossRef - Breast Cancer and Exposure to Organochlorines in the CECILE Study: Associations with Plasma Levels Measured at the Time of Diagnosis and Estimated during Adolescence
Delphine Bachelet, Marc-André Verner, Monica Neri, Émilie Cordina Duverger, Corinne Charlier, Patrick Arveux, Sami Haddad, Pascal Guénel
International Journal of Environmental Research an.2019; 16(2): 271. CrossRef - Risk of breast cancer and adipose tissue concentrations of polychlorinated biphenyls and organochlorine pesticides: a hospital-based case-control study in Chinese women
Wenlong Huang, Yuanfang He, Jiefeng Xiao, Yuanni Huang, Anna Li, Meirong He, Kusheng Wu
Environmental Science and Pollution Research.2019; 26(31): 32128. CrossRef - Serum levels of Organochlorine Pesticides and Breast Cancer Risk in Iranian Women
Parisa Paydar, Gholamreza Asadikaram, Hossein Fallah, Hamid Zeynali Nejad, Hamed Akbari, Moslem Abolhassani, Vahid Moazed, Payam Khazaeli, Mahmoud Reza Heidari
Archives of Environmental Contamination and Toxico.2019; 77(4): 480. CrossRef - DDT exposure in early childhood and female breast cancer: Evidence from an ecological study in Taiwan
Simon Chang, Sonia El-Zaemey, Jane Heyworth, Meng-chi Tang
Environment International.2018; 121: 1106. CrossRef - Chiral pharmaceuticals: Environment sources, potential human health impacts, remediation technologies and future perspective
Yaoyu Zhou, Shikang Wu, Hao Zhou, Hongli Huang, Jia Zhao, Yaocheng Deng, Hua Wang, Yuan Yang, Jian Yang, Lin Luo
Environment International.2018; 121: 523. CrossRef - Organochlorine pesticides accumulation and breast cancer: A hospital-based case–control study
Ting-Ting He, An-Jun Zuo, Ji-Gang Wang, Peng Zhao
Tumor Biology.2017; 39(5): 101042831769911. CrossRef - Correlation between toxic organochlorine pesticides and breast cancer
SA Eldakroory, DA El Morsi, RH Abdel-Rahman, S Roshdy, MS Gouida, EO Khashaba
Human & Experimental Toxicology.2017; 36(12): 1326. CrossRef - Breast cancer and persistent organic pollutants (excluding DDT): a systematic literature review
Tafzila Akter Mouly, Leisa-Maree Leontjew Toms
Environmental Science and Pollution Research.2016; 23(22): 22385. CrossRef
- Causes and Risk Factors of Breast Cancer, What Do We Know for Sure? An Evidence Synthesis of Systematic Reviews and Meta-Analyses
- Seroepidemiology of Hepatitis A Infection in Northeastern China, Korea, and Japan
- Haesun Yun, Hyeok-Jin Lee, Youngsil Yoon, Kisang Kim, Sungsoo Kim, Myung-Hee Shin, Miyuki Taniguchi, Soo Ryang Kim, Mi Kyung Kim
- Osong Public Health Res Perspect. 2012;3(1):31-35. Published online December 31, 2011
- DOI: https://doi.org/10.1016/j.phrp.2012.01.005
- 2,776 View
- 13 Download
- 5 Crossref
-
 Abstract
Abstract
 PDF
PDF - Objectives
The epidemiological patterns of endemic hepatitis A virus (HAV) are unclear in northeastern Asia depending on the ethnicity of the country in question. The purpose of this study was to investigate the seroprevalence of HAV in northeastern China, South Korea, and Japan.
Methods
A total of 1,500 serum samples were collected from five groups of inhabitants (300 each) who were over 40 years of age (Korean Chinese, indigenous Chinese, South Korean, Korean living in Japan, and indigenous Japanese). The samples were screened for antibodies to HAV using an enzyme-linked immunosorbent assay.
Results
Positivity for HAV antibodies was 93.7% (95% confidence interval [CI]: 90.9–96.4) in Koreans living in northeastern China, 99.7% (95% CI: 99.0–100.3) in indigenous Chinese, 98.0% (95% CI: 96.4–99.6) in indigenous Koreans, 33.3% (95% CI: 28.0–38.7) in Koreans living in Japan, and 20.4% (95% CI: 15.8–25.0) in indigenous Japanese persons. The overall anti-HAV prevalence was not significantly different between northeastern China and South Korea, but it was different in Japan.
Conclusions
These results indicate that differences in seroprevalence can be attributed to geological, environmental, and socioeconomic conditions rather than ethnicity. -
Citations
Citations to this article as recorded by- Prevalence of Anti-Hav IgG Antibodies in the Population of the Łódź Macroregion by Age Group
Gabriela Henrykowska, Kornelia Kotecka, Aleksandra Jabłkowska, Andrzej Buczyński, Joanna Woźny
Polish Hyperbaric Research.2021; 76(3): 67. CrossRef - Sero-prevalence of viral hepatitis A in a district of Sri Lanka: a community based cross-sectional study
Nalin Ariyarathna, Chrishantha Abeysena
BMC Infectious Diseases.2019;[Epub] CrossRef - Seroprevalence of Hepatitis A among Children and Young Adults Residing in Tehran, Iran: Implication for HAV Vaccination
Amitis Ramezani, Mohammad Reza Aghasadeghi, Setareh Mamishi, Shahram Sabeti, Farahnaz Bidari - Zerehpoosh, Mohammad Banifazl, Anahita Bavand, Sahar Shadanlou, Arezoo Aghakhani
Hepatitis Monthly.2018;[Epub] CrossRef - Seroepidemiology of Hepatitis Viruses and Hepatitis B Genotypes of Female Marriage Immigrants in Korea
Jae-Cheol Kwon, Hye Young Chang, Oh Young Kwon, Ji Hoon Park, In Soo Oh, Hyung Joon Kim, Jun Hyung Lee, Ha-Jung Roh, Hyun Woong Lee
Yonsei Medical Journal.2018; 59(9): 1072. CrossRef - Seroprevalence of Helicobacter pylori and Hepatitis A Virus among Children in Rural Central Taiwan
Meng-Che Wu, Chia-Hsing Sung, Yu-Chuan Chang, Chi-Lin Ho, Chih-Chiang Wu, Kuei-Hua Wu, Chun-Yi Lee, Kuen-Der Yang
Japanese Journal of Infectious Diseases.2015; 68(6): 494. CrossRef
- Prevalence of Anti-Hav IgG Antibodies in the Population of the Łódź Macroregion by Age Group
- Seroprevalence of Hepatitis A and E Viruses Based on the Third Korea National Health and Nutrition Survey in Korea
- Haesun Yun, Hyeok-Jin Lee, Doosung Cheon, Chaeshin Chu, Kyung Won Oh, Young Taek Kim, Youngmee Jee
- Osong Public Health Res Perspect. 2011;2(1):46-50. Published online June 30, 2011
- DOI: https://doi.org/10.1016/j.phrp.2011.04.009
- 3,050 View
- 16 Download
- 7 Crossref
-
 Abstract
Abstract
 PDF
PDF - Objectives
The purpose of this study was to investigate the seroprevalence of hepatitis A virus (HAV) and hepatitis E virus (HEV) in Korea during 2005.
Methods
Study subjects were selected from across Korea using a stratified multistage probability sampling design, and HAV and HEV seroprevalence was compared on the basis of sex, age, and residency. A total of 497 rural and urban people aged 10–99 years of age (mean ± SD age = 28.87 ± 17.63 years) were selected by two-stage cluster sampling and tested serologically for anti-HAV and anti-HEV IgG using an enzyme-linked immunosorbent assay.
Results
Among this population, the overall seroprevalence of HAV was 63.80% (55.21% aged in their 20s and 95.92% in their 30s, p < 0.01) and that of HEV was 9.40% (5.21% aged in their 20s and 7.14% in their 30s, p < 0.01). Seroprevalence also varied according to area of residence. HEV prevalence in rural areas was higher than that of urban regions based on the anti-HEV antibody, odds ratio 3.22 (95% confidence interval: 1.46–7.10, p < 0.01). There were no significant differences between male and female against anti-HAV/HEV antibodies.
Conclusion
Our study suggested that the seropositive rates of HAV and HEV might be related to age and environmental conditions. -
Citations
Citations to this article as recorded by- Factors associated with anti-hepatitis A virus immunoglobulin G seropositivity among Korean workers: a cross-sectional study
Eunchan Mun, Yesung Lee, Byungseong Suh, Wonsul Kim, Jinsook Jeong, Hwanjin Park, Woncheol Lee, Boksoon Han, Soyoung Park, Changhwan Lee
BMJ Open.2020; 10(6): e036727. CrossRef - Seroprevalence and risk factors of hepatitis E virus infection among the Korean, Manchu, Mongol, and Han ethnic groups in Eastern and Northeastern China
Yanan Cai, Si-Yuan Qin, Aidong Qian, Peng Xu, Ying-Tian Xu, Lin-Hong Xie, Quan Zhao, Xiao-Xuan Zhang
Journal of Medical Virology.2017; 89(11): 1988. CrossRef - Hepatitis E virus exposure in pregnant women in rural Durango, Mexico
Cosme Alvarado-Esquivel, Luis F. Sánchez-Anguiano, Jesús Hernández-Tinoco
Annals of Hepatology.2014; 13(5): 510. CrossRef - Epidemiologic Study on Hepatitis A Virus Seroprevalence in Busan
Kyung-Soon Cho, So-Hyun Park
Korean Journal of Clinical Laboratory Science.2014; 46(1): 17. CrossRef - A Systematic Review of Hepatitis E Virus Infection in Children
V. P. Verghese, J. L. Robinson
Clinical Infectious Diseases.2014; 59(5): 689. CrossRef - Hepatitis E Virus (HEV) Seroprevalence in the general population of the Republic of Korea in 2007–2009: a nationwide cross-sectional study
Youngsil Yoon, Hye Sook Jeong, Haesun Yun, Hyeokjin Lee, Yoo-Sung Hwang, Bohyun Park, Chae Jin Lee, Sangwon Lee, Ji-Yeon Hyeon
BMC Infectious Diseases.2014;[Epub] CrossRef - The Road Less Traveled
Chaeshin Chu
Osong Public Health and Research Perspectives.2011; 2(1): 1. CrossRef
- Factors associated with anti-hepatitis A virus immunoglobulin G seropositivity among Korean workers: a cross-sectional study
- Trends in Water- and Foodborne Disease Outbreaks in Korea, 2007–2009
- Jin Gwack, Kyoung-Chan Lee, Hyo Jin Lee, Wooseok Kwak, Dong Woo Lee, Yeon Hwa Choi, Jin Seok Kim, Young Ah Kang
- Osong Public Health Res Perspect. 2010;1(1):50-54. Published online December 31, 2010
- DOI: https://doi.org/10.1016/j.phrp.2010.12.011
- 3,172 View
- 18 Download
- 17 Crossref
-
 Abstract
Abstract
 PDF
PDF - Objectives
In Korea, every outbreak of acute gastroenteritis in two or more patients who are epidemiologically related is investigated by local public health centres to determine causative agents and control the outbreak with the support of the Korean Centers for Disease Control and Prevention. The findings and conclusions of each outbreak investigation have been summarized annually since 2007 to make reports and statistics of water- and foodborne disease outbreaks.
Methods
All outbreaks reported to Korean Centers for Disease Control and Prevention from 2007 to 2009 were included in the study. We analysed the trends and epidemiologic aspects of outbreaks by month, year, and location.
Results
The total number of outbreaks decreased steadily each year for the period the study covered, whereas the number of patients per outbreak continued to increase resulting from a dramatic increase in the number of patients per outbreak in food service establishments. The outbreaks occurred in the period of June to September, when temperature and humidity are relatively high, which accounted for 44.3% of total outbreaks. The monthly number of outbreaks decreased steadily until November after peaking in May 2009. The most common causative agent was norovirus (16.5%) followed by pathogenic Escherichia coli. The rate of causative agent identification was 60.1%, with higher identification rates in larger outbreaks.
Conclusions
Although a decreasing trend of outbreaks by year was observed in the study, the food services in schools and companies require more attention to hygiene and sanitation to prevent large outbreaks. The ability to establish the cause of an outbreak should be further improved. -
Citations
Citations to this article as recorded by- 2023년 하절기 수인성ㆍ식품매개감염병 비상방역 체계 운영 결과
성찬 양, 소연 박, 선경 박, 지수 원, 형준 김, 진선 양
Public Health Weekly Report.2024; 17(4): 149. CrossRef - Prevalence of Salmonella spp. and Escherichia coli in the feces of free-roaming wildlife throughout South Korea
Rahman M. Mafizur, Lim Sangjin, Park Y. Chul, Csaba Varga
PLOS ONE.2024; 19(2): e0281006. CrossRef - 2022년 하절기 수인성 및 식품매개감염병 비상방역체계 운영결과
다슬 김, 인호 김, 형준 김, 지애 심, 지수 원, 진 곽
Public Health Weekly Report.2023; 16(2): 36. CrossRef - Trends in recent waterborne and foodborne disease outbreaks in South Korea, 2015–2019
Sang Hyuk Lee, Jae-Won Yun, Ji Hee Lee, Yeon Haw Jung, Dong Han Lee
Osong Public Health and Research Perspectives.2021; 12(2): 73. CrossRef - Nationwide surveillance on serotype distribution and antimicrobial resistance profiles of non-typhoidal Salmonella serovars isolated from food-producing animals in South Korea
Abraham Fikru Mechesso, Dong Chan Moon, Su-Jeong Kim, Hyun-Ju Song, Hee Young Kang, Seok Hyeon Na, Ji-Hyun Choi, Ha-Young Kim, Soon-Seek Yoon, Suk-Kyung Lim
International Journal of Food Microbiology.2020; 335: 108893. CrossRef - Development of an HTS system to identify natural chemicals that specifically inhibit Escherichia coli O157:H7 adhesion to host cells
Seung Min Kim, Hyun Jung Kim
Food Control.2017; 73: 185. CrossRef - Epidemiological relationships of Campylobacter jejuni strains isolated from humans and chickens in South Korea
Jae-Young Oh, Yong-Kuk Kwon, Bai Wei, Hyung-Kwan Jang, Suk-Kyung Lim, Cheon-Hyeon Kim, Suk-Chan Jung, Min-Su Kang
Journal of Microbiology.2017; 55(1): 13. CrossRef - A large outbreak of acute gastroenteritis caused by the human norovirus GII.17 strain at a university in Henan Province, China
Xue-Yong Huang, Jia Su, Qian-Chao Lu, Shi-Zheng Li, Jia-Yong Zhao, Meng-Lei Li, Yi Li, Xiao-Jing Shen, Bai-Fan Zhang, Hai-Feng Wang, Yu-Jiao Mu, Shu-Yu Wu, Yan-Hua Du, Li-Cheng Liu, Wei-Jun Chen, John David Klena, Bian-Li Xu
Infectious Diseases of Poverty.2017;[Epub] CrossRef - Consecutive Outbreaks of EnterotoxigenicEscherichia coliO6 in Schools in South Korea Caused by Contamination of Fermented Vegetable Kimchi
Jaeseung Shin, Ki-Bok Yoon, Doo-Young Jeon, Sung-Suk Oh, Kyung-Hwan Oh, Gyung Tae Chung, Seung Woo Kim, Seung-Hak Cho
Foodborne Pathogens and Disease.2016; 13(10): 535. CrossRef - Prevalence and characterization of Salmonella in pigs from conventional and organic farms and first report of S. serovar 1,4,[5],12:i:- from Korea
Migma Dorji Tamang, Mamata Gurung, Hyang-Mi Nam, Dong Chan Moon, Su-Ran Kim, Geum-Chan Jang, Dae-Yeong Jung, Suk-Chan Jung, Yong-Ho Park, Suk-Kyung Lim
Veterinary Microbiology.2015; 178(1-2): 119. CrossRef - First norovirus outbreaks associated with consumption of green seaweed (Enteromorpha spp.) in South Korea
J. H. PARK, H. S. JEONG, J. S. LEE, S. W. LEE, Y. H. CHOI, S. J. CHOI, I. S. JOO, Y. R. KIM, Y. K. PARK, S. K. YOUN
Epidemiology and Infection.2015; 143(3): 515. CrossRef - Antimicrobial Susceptibility and Virulence Characteristics of Salmonella enterica Typhimurium Isolates from Healthy and Diseased Pigs in Korea
Migma Dorji Tamang, Mamata Gurung, Hyang-Mi Nam, Dong Chan Moon, Geum-Chan Jang, Suk-Chan Jung, Suk-Kyung Lim
Journal of Food Protection.2014; 77(9): 1481. CrossRef - Emerging Pathogens and Vehicles of Food- and Water-borne Disease Outbreaks in Korea, 2007–2012
Shinje Moon, Il-Woong Sohn, Yeongseon Hong, Hyungmin Lee, Ji-Hyuk Park, Geun-Yong Kwon, Sangwon Lee, Seung-Ki Youn
Osong Public Health and Research Perspectives.2014; 5(1): 34. CrossRef - Diarrheal Outbreak Caused by Atypical EnteropathogenicEscherichia coliO157:H45 in South Korea
Ji-Hyuk Park, Sung-Suk Oh, Kyung-Hwan Oh, Jaeseung Shin, Eun Jung Jang, Byung-Yool Jun, Seung-Ki Youn, Seung-Hak Cho
Foodborne Pathogens and Disease.2014; 11(10): 775. CrossRef - Efficiency of fractionated γ-irradiation doses to eliminate vegetative cells and spores of Bacillus cereus from raw rice
Adelard B. Mtenga, Neema Kassim, Won-Bo Shim, Duck-Hwa Chung
Food Science and Biotechnology.2013; 22(2): 577. CrossRef - Norovirus Contamination Levels in Ground Water Treatment Systems Used for Food-Catering Facilities in South Korea
Bo-Ram Lee, Sung-Geun Lee, Jong-Hyun Park, Kwang-Yup Kim, Sang-Ryeol Ryu, Ok-Jae Rhee, Jeong-Woong Park, Jeong-Su Lee, Soon-Young Paik
Viruses.2013; 5(7): 1646. CrossRef - A review of microbial biofilms of produce: Future challenge to food safety
Iqbal Kabir Jahid, Sang-Do Ha
Food Science and Biotechnology.2012; 21(2): 299. CrossRef
- 2023년 하절기 수인성ㆍ식품매개감염병 비상방역 체계 운영 결과



 First
First Prev
Prev


